
Want to reduce your risk of dementia? Get your hearing checked today

Are you having a little trouble hearing conversations? If so, you’re not alone. An estimated 23% of Americans ages 12 and older have hearing loss. Although most of those people have mild hearing loss, for people ages 80 years and older, it’s more common for hearing loss to be moderate to severe than mild.
But not only is moderate to severe hearing loss disruptive to one’s life, it also makes you more likely to develop dementia. A new study helps explain why — and what you can do about it.
What did the new study look at and find?
A study published in JAMA focused on a sample of adults in the United States from the National Health and Aging Trends Study, which follows Medicare beneficiaries. The participants sampled were 70 or older.
The researchers found that about 33% of participants had normal hearing, 37% had mild hearing loss, and 30% had moderate to severe hearing loss. Dementia occurred least often among those with normal hearing (6%), more often among those with mild hearing loss (9%), and most often among those with moderate to severe hearing loss (17%). That’s a large increase in risk, particularly for those whose hearing loss is moderate to severe.
What else to know about this study
The study sample was selected to make it possible to analyze subgroups by age and apply findings to a diverse population. The sample included additional participants ages 90 years and older, and additional participants who identified as Black. Of the 2,413 total participants, 53% were ages 80 years and older, 56% were female, 19% were non-Hispanic Black, 4.5% were Hispanic, and 74% were non-Hispanic white.
Also, unlike previous research, this study looked objectively at hearing loss and dementia. Prior research had shown that hearing loss is thought to account for about 8% of all dementia cases worldwide. Exactly why the connection exists is not known.
It’s important to note that most large studies that found this link were based on questionnaires that people fill out. In other words, no one actually measured the hearing of those participating in the study to make sure that they had hearing loss — or that their hearing was really normal.
In this new study, however, the investigative team used an electronic tablet-based audiometer to evaluate participants’ hearing for four pure tone frequencies that are most important for understanding speech. So, for the first time in a large study, there was objective measurement of hearing loss.
How do hearing aids reduce the risk of dementia?
If you have hearing loss, does that mean you’re doomed to develop dementia? Not at all. This study found that those with moderate to severe hearing loss could significantly reduce their risk of dementia simply by using hearing aids.
This research helps us understand why hearing loss causes dementia. Here’s the connection:
There is increasing evidence that the more the brain is stimulated, the less likely it is that dementia will develop. When there is hearing loss, auditory stimulation is reduced. This, by itself, likely increases dementia risk. But even more important is that when an individual suffers from moderate to severe hearing loss, they are less likely to participate in social activities. Perhaps they are embarrassed about their hearing loss. Or they may simply find it unrewarding to attend a social event when they cannot hear what is going on.
It turns out that social activities are one of the best ways to stimulate the brain, as there is evidence that our brains evolved to facilitate social behavior. Given all this information, you won’t be surprised to learn that reduced social activity has been linked to cognitive decline. Thus, this new study provides additional evidence that the reason hearing loss increases the risk of dementia is because hearing loss reduces brain stimulation — both directly and through reduced social interaction.
What to do if you have hearing loss
Don’t let hearing loss raise your risk of dementia.
- Keep your ears clean. (But remember, never put anything in your ears smaller than your elbow. Ask your doctor if you’re not sure how to clean your ears.)
- If you can’t hear and you don’t have hearing aids, get them. Hearing aids now available over the counter can help many people with mild to moderate hearing loss.
- If you have hearing aids, wear them.
- If your hearing aids aren’t working, get them fixed.
- Don’t be passive — ramp up your social life and other activities.
All these things will help to reduce your risk of dementia. And you might just find that, despite some hearing loss, you’re enjoying life more.
About the Author
Andrew E. Budson, MD, Contributor; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Andrew E. Budson is chief of cognitive & behavioral neurology at the Veterans Affairs Boston Healthcare System, lecturer in neurology at Harvard Medical School, and chair of the Science of Learning Innovation Group at the … See Full Bio View all posts by Andrew E. Budson, MD
Veins are a key player in the body: Here’s why
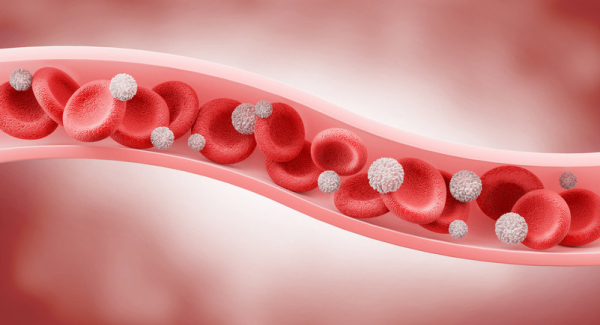
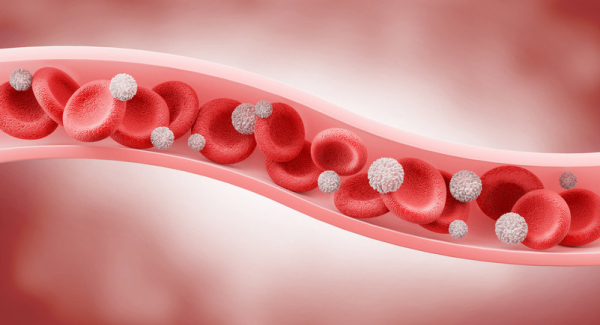
Blood circulation is vital to our health. Our arteries deliver oxygen, energy-rich nutrients, hormones, immune cells, and other essentials throughout the body. When deliveries are cut off, organs and tissue can be irreversibly damaged within minutes.
But a second part of blood circulation is also vitally important: the return trip. After our arteries deliver the goods, our blood must return to the lungs to pick up more oxygen, stock up on nutrients, get rid of carbon dioxide, and head back to the heart to be pumped out again. In this way, blood is in continuous motion, ensuring organs and tissues get what they need while waste products are removed.
The vessels designed for the return trip are your veins. Read on for answers to questions about how veins work, what can interfere with their ability to work smoothly, and five ways to keep thousands of miles of these blood vessels healthy.
What are veins and what do they do?
Perhaps you haven't thought much about your veins. Or if you have, maybe you focused on varicose veins, those swollen, unsightly purplish vessels that may be visible just beneath the skin of the legs. Or perhaps you had a blood test and the person taking the blood had a hard time finding a "good vein." But these are just a small part of vein world.
Veins make up a network of connecting tubes throughout the human body, ranging in size from 1 mm (about the size of a pencil point) to 2 cm (about the size of a quarter), that bring blood low in oxygen back to the lungs to reload with oxygen. Then four pulmonary veins carry oxygen-rich blood from the lungs to the heart. (Fun fact: some people have three or five pulmonary veins, but most of us have four.)
Often, major veins are found alongside similarly named arteries, like a highway with cars moving in opposite directions: in the upper arm, for example, the axillary vein lies next to the axillary artery; in the kidney, the renal vein runs alongside the renal artery.
How do veins help keep blood flowing?
Let's start by picturing tiny red blood cells loaded up with oxygen. Now imagine you're a red blood cell that has just traveled from the heart through the arteries to a calf muscle of someone who is jogging. After you drop off the much-needed oxygen and pick up waste products like carbon dioxide, you need to get back to the heart — fast! — because exercising muscles need extra oxygen.
But wait. As you head back to the lungs to load up on more oxygen and release carbon dioxide, there's a steep climb straight up. How can you make it back to the lungs without help?
Fortunately, veins have tiny valves within them that allow blood to flow in only one direction. When muscles contract near larger veins, they pump blood toward the lungs. In addition, taking in a breath creates a sort of suction that pulls blood toward the lungs. Without these forces encouraging blood to flow in the right direction through the veins, blood flowing into the legs would pool there, causing dangerously high pressure and swelling.
Why are veins blue?
Actually, they aren't. People think they're blue because that's often how they appear in diagrams and illustrations. But that's just to set them apart from the bright red arteries.
The veins on the back of your hand may appear blue if you have light-colored skin. That's an illusion due to the way light is absorbed by the skin. In people with darker skin tones, veins tend to blend in more.
If you could look at veins directly, without any skin in the way, they'd appear pale because they are naturally colorless, or dark red due to the blood inside them.
What sort of problems can occur in veins?
Blood clots, varicose veins, and venous insufficiency are some of the most common health conditions affecting the veins:
- Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, blocking blood flow. This condition is potentially serious because clots in deep veins can travel to the lungs, causing a life-threatening pulmonary embolism by blocking an artery that delivers blood to part of the lungs.
- Superficial thrombophlebitis is a blood clot in a small vein just under the skin. This causes inflammation and pain.
- Varicose veins are small veins under the skin that swell and twist. While these may be harmless, they can cause pain and are occasionally complicated by blood clots.
- Venous insufficiency occurs when the valves in veins are damaged — due to aging or prior blood clots, for example. The blood flow through the veins may be impaired, leading to leg swelling, increased pressure, inflamed skin, and poor healing.
One far more rare condition goes by the impressive name of phlegmasia cerulea dolens. It is a serious complication of DVT in which the obstruction of blood flow through a deep vein leads to blocked blood flow through nearby arteries. That can cause gangrene and the need for amputation.
All of these conditions can affect circulation temporarily or in a lasting way. Treatments are aimed at restoring circulation, if possible.
Top 5 ways to improve vein health
Healthy veins help the heart, brain, and every other part of your body. Here are five ways to improve vein health, even if you already have vein disease:
- Be active. Exercise regularly and avoid prolonged standing or sitting.
- Choose healthy foods, such as those in a plant-based, heart-healthy diet.
- Maintain a healthy weight.
- Don't smoke.
- Wear compression stockings if you already have vein disease such as venous insufficiency.
And of course, seek medical care for unexplained swelling, inflammation, or ulcers on your legs, ankles, or feet.
The bottom line
Our veins are busy around the clock, shuttling blood from distant sites back to the lungs and heart, which pumps enriched blood out again. Without veins, blood circulation could not happen. They're a good example of how many parts of your amazing body are easy to overlook until something goes wrong.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD